Abstract
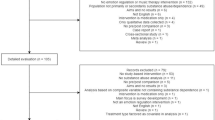
Methadone maintenance treatment (MMT) is a common drug treatment for opioid dependence disorder. This treatment, with positive results, has many physical and psychological complications. The purpose of this study was to evaluate the effectiveness of dialectical behavioral therapy (DBT) on emotional regulation, distress tolerance, craving, and depression in patients under MMT. The present study was a randomized controlled clinical trial with two groups of intervention (MMT with Dialect-Behavioral Therapy (DBT)) and control group (MMT). Initial evaluations were performed by clinical psychiatrist at the clinic. 50 men who referred to the methadone treatment clinic were randomly assigned to two groups of the present study. The research data were collected from demographic information form, Structured Clinical Interview for Axis I Disorders, emotion regulation questionnaire, distress tolerance questionnaire, Instant craving questionnaire, and Beck Depression Inventory in three stages: pre-test, post-test and three-month follow-up. Statistical analysis was performed using Kolmogorov–Smirnov test, Lion test, Chi-square, T-test and repeated measures. The findings showed that MMT + DBT significantly improved emotion regulation and distress tolerance in post-test and 3 months follow-up, and significantly reduced craving and depression. The simultaneous combination of MMT with DBT can be helpful in reducing the psychological problems of opiate dependent people under MMT. Given the emphasis on dialectical behavioral therapy on emotion regulation as the main mechanism of change, this therapy can be a useful treatment for other psychological disorders that are involved with emotional problems.

Similar content being viewed by others
References
Afshari, B. (2020). Personality and anxiety disorders: Examination of revised reinforcement sensitivity theory in clinical generalized anxiety disorder, social anxiety disorder, and panic disorder. Current Issues in Personality Psychology, 8(1), 52–60.
Afshari, B., & Hasani, J. (2020). Study of dialectical behavior therapy versus cognitive behavior therapy on emotion regulation and mindfulness in patients with generalized anxiety disorder. Journal of Contemporary Psychotherapy, 50, 305–312.
Afshari, B., Khezrian, K., & Faghihi, A. (2019). Examination and comparison of cognitive and executive functions in patients with schizophrenia and bipolar disorders. Journal of Isfahan Medical School. https://doi.org/10.22122/jims.v37i320.11149
Afshari, B., Omidi, A., & Ahmadvand, A. (2019). Effects of dialectical behavior therapy on executive functions, emotion regulation, and mindfulness in bipolar disorder. Journal of Contemporary Psychotherapy. https://doi.org/10.1007/s10879-019-09442-7.
Afshari, B., Rasouli-Azad, M., & Ghoreishi, F. S. (2019). Comparison of original and revised reinforcement sensitivity theory in clinically-stable schizophrenia and bipolar disorder patients. Personality and Individual Differences, 138, 321–327.
Aghasi, A., & Atashpour, S. (2017). The impact of dialectical behavior therapy-based intervention on craving men with addiction disorders (opioid-methamphetamine). Community Health Journal, 10(2), 11–23.
Aghataher, A., & Mahani, K. N. J. B. (2014). The effect of rational emotive behavior group therapy on self-concept and depression of self-introduced drug abusers referred to Ofogh Addiction Treatment Center in Zarand (Kerman, Iran). Biomedical and Pharmacology Journal, 7(1), 317–323.
Alexander, A. C., & Ward, K. D. (2018). Understanding postdisaster substance use and psychological distress using concepts from the self-medication hypothesis and social cognitive theory. Journal of Psychoactive Drugs, 50(2), 177–186.
Bass, S. B., Jessop, A., Maurer, L., Gashat, M., Al Hajji, M., & Gutierrez, M. (2018). Mapping the barriers and facilitators of HCV treatment initiation in methadone maintenance therapy patients: Implications for intervention development. Journal of Health Communication, 23(1), 117–127.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Beck depression inventory-II (Vol. 78, No. 2, pp. 490–498). San Antonio.
Beckstead, D. J., Lambert, M. J., DuBose, A. P., & Linehan, M. (2015). Dialectical behavior therapy with American Indian/Alaska Native adolescents diagnosed with substance use disorders: Combining an evidence based treatment with cultural, traditional, and spiritual beliefs. Addictive Behaviors, 51, 84–87.
Bohus, M., Haaf, B., Stiglmayr, C., Pohl, U., BoÈhme, R., & Linehan, M. (2000). Evaluation of inpatient dialectical-behavioral therapy for borderline personality disorder—a prospective study. Behaviour Research and Therapy, 38(9), 875–887.
Bowen, S., Somohano, V. C., Rutkie, R. E., Manuel, J. A., & Rehder, K. L. (2017). Mindfulness-based relapse prevention for methadone maintenance: A feasibility trial. Journal of Alternative and Complementary Medicine, 23(7), 541–544.
Chowdhury, N., Kevorkian, S., Hawn, S. E., Amstadter, A. B., Dick, D., Kendler, K. S., & Berenz, E. C. (2018).Associations between personality and distress tolerance among trauma-exposed young adults. Personality and Individual Differences, 120, 166–170.
Coyle, T. N., Shaver, J. A., & Linehan, M. M. (2018). On the potential for iatrogenic effects of psychiatric crisis services: The example of dialectical behavior therapy for adult women with borderline personality disorder. Journal of Consulting and Clinical Psychology, 86(2), 116.
Dingle, G. A., da Costa Neves, D., Alhadad, S. S., & Hides, L. (2018). Individual and interpersonal emotion regulation among adults with substance use disorders and matched controls.The British Journal of Clinical Psychology, 57(2), 186–202.
El Hage, C., Ghabrash, M. F., Dubreucq, S., Brissette, S., Lespérance, F., Lespérance, P., … Jutras-Aswad, D. (2018). A pilot, open-label, 8-week study evaluating desvenlafaxine for treatment of major depression in methadone-maintained individuals with opioid use disorder. International Clinical Psychopharmacology. 33(5), 268–273.
Farnia, V., Alikhani, M., Ebrahimi, A., Golshani, S., Bahmani, D. S., & Brand, S. (2019). Ginseng treatment improves the sexual side effects of methadone maintenance treatment. Psychiatry Research, 276, 142–150.
First, M. B., Spitzer, R. L., Gibbon, M., & Williams, J. B. (1995). The structured clinical interview for DSM-III-R personality disorders (SCID-II). Part I: Description. Journal of Personality Disorders, 9(2), 83–91.
Franken, I. H., Hendriks, V. M., & van den Brink, W. (2002). Initial validation of two opiate craving questionnaires: The Obsessive Compulsive Drug Use Scale and the Desires for Drug Questionnaire. Addictive Behavior, 27(5), 675–685.
Grant, B. F., Hasin, D. S., Stinson, F. S., Dawson, D. A., Chou, S. P., Ruan, W. J., & Huang, B. (2005). Co-occurrence of 12-month mood and anxiety disorders and personality disorders in the US: results from the national epidemiologic survey on alcohol and related conditions. Journal of Psychiatric Research, 39(1), 1–9.
Hasani, J. (2016). Persian version of the emotion regulation questionnaire: Factor structure, reliability and validity. International Journal of Behavioral Sciences, 10(3), 156–161.
Hassan, A., Bhatia, S. K., & Bhatia, S. C. (2017). Cognitive-behavioral therapy and other psychosocial interventions for substance use disorders. Substance and Non Substance Related Addiction Disorders: Diagnosis and Treatment, 16, 227–242.
Hayati, K. (2020). Psychometric properties of malay-translated version of “Desire for Drug Questionnaire” among opioid dependents. International Journal of Public Health and Clinical Sciences, 7(2), 40–50.
Hensley, L., Sulo, S., Kozmic, S., & Parilla, B. V. (2018). Opioid addiction in pregnancy: Does depression negatively impact adherence with prenatal care? Journal of Addiction Medicine, 12(1), 61–64.
Hunt, G. E., Large, M. M., & Cleary, M. (2020). Prevalence of comorbid substance use in major depressive disorder in community and clinical settings, 1990–2019: Systematic review and meta-analysis. Journal of Affective Disorders. https://doi.org/10.1016/j.jad.2020.01.141.
Jalali, A., Yekzaman, M., Bazrafshan, M.-R., Salari, N., & Rahmati, M. (2018). Investigating the effect of family counseling on the acceptance and support of patients under methadone maintenance treatment. Shiraz E-Medical Journal, 19(5), e62347.
John, O. P., & Gross, J. J. (2004). Healthy and unhealthy emotion regulation: Personality processes, individual differences, and life span development. Journal of Personality, 72(6), 1301–1334.
Karow, A., Reimer, J., Schäfer, I., Krausz, M., Haasen, C., & Verthein, U. (2010). Quality of life under maintenance treatment with heroin versus methadone in patients with opioid dependence. Drug and Alcohol Dependence, 112(3), 209–215.
Kessel, J. B., Castel, L. D., & Nemecek, D. A. J. A. J. P. B. (2018). Clinical and cost outcomes of buprenorphine treatment in a commercial benefit plan population. American Journal of Pharmacy Benefits, 10, 84–89.
Kiluk, B. D., DeVito, E. E., Buck, M. B., Hunkele, K., Nich, C., & Carroll, K. M. (2017). Effect of computerized cognitive behavioral therapy on acquisition of coping skills among cocaine-dependent individuals enrolled in methadone maintenance. Journal of Substance Abuse Treatment, 82, 87–92.
Kuo, H.-W., Liu, T.-H., Tsou, H.-H., Hsu, Y.-T., Wang, S.-C., Fang, C.-P., … Liu, Y.-L. (2018). Inflammatory chemokine eotaxin-1 is correlated with age in heroin dependent patients under methadone maintenance therapy. Drug and Alcohol Dependence, 183, 19–24.
Lau, M. A., & McMain, S. F. (2005). Integrating mindfulness meditation with cognitive and behavioural therapies: The challenge of combining acceptance-and change-based strategies. Canadian Journal of Psychiatry, 50(13), 863–869.
Linehan, M. M., Armstrong, H. E., Suarez, A., Allmon, D., & Heard, H. L. (1991). Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Archives of General Psychiatry, 48(12), 1060–1064.
Linehan, M. M., Heard, H. L., & Armstrong, H. E. (1993). Naturalistic follow-up of a behavioral treatment for chronically parasuicidal borderline patients. Archives of General Psychiatry, 50(12), 971–974.
Linehan, M. M., Korslund, K. E., Harned, M. S., Gallop, R. J., Lungu, A., Neacsiu, A. D., & Murray-Gregory, A. M. (2015). Dialectical behavior therapy for high suicide risk in individuals with borderline personality disorder: A randomized clinical trial and component analysis. JAMA Psychiatry, 72(5), 475–482.
Marceau, E. M., Kelly, P. J., & Solowij, N. (2018). The relationship between executive functions and emotion regulation in females attending therapeutic community treatment for substance use disorder. Drug and Alcohol Dependence, 182, 58–66.
Mattick, R. P., Breen, C., Kimber, J., & Davoli, M. (2014). Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database System Review, 2004(3), CD002207.
Meygoni, A. K. M., & Ahadi, H. (2012). Declining the rate of major depression: Effectiveness of dialectical behavior therapy. Procedia-Social and Behavioral Sciences, 35, 230–236.
Moore, K. E., Oberleitner, L., Smith, K. M., Maurer, K., & McKee, S. A. (2018). Feasibility and effectiveness of continuing methadone maintenance treatment during incarceration compared with forced withdrawal. Journal of Addiction Medicine, 12(2), 156–162.
Mulkens, S., de Vos, C., de Graaff, A., & Waller, G. (2018). To deliver or not to deliver cognitive behavioral therapy for eating disorders: Replication and extension of our understanding of why therapists fail to do what they should do. Behaviour Research and Therapy, 106, 57–63.
Nyamathi, A. M., Shin, S. S., Smeltzer, J., Salem, B. E., Yadav, K., Ekstrand, M. L., … Faucette, M. (2017). Achieving drug and alcohol abstinence among recently incarcerated homeless women: A randomized controlled trial comparing dialectical behavioral therapy-case management with a health promotion program. Nursing Research, 66(6), 432–441.
Otaghsara, S. R. (2006). The relative efficiency of public and non-public health centres in Iran. University of Keele.
Owens, M. D., Nason, E., & Yeater, E. (2018). Dialectical behavior therapy for multiple treatment targets: A case study of a male with comorbid personality and substance use disorders. International Journal of Mental Health and Addiction, 16(2), 436–450.
Prosek, E. A., Giordano, A. L., Woehler, E. S., Price, E., & McCullough, R. (2018). Differences in emotion dysregulation and symptoms of depression and anxiety among illicit substance users and nonusers. Substance Use & Misuse, 53(11), 1915–1918.
Rahmani, M., Omidi, A., Asemi, Z., & Akbari, H. (2018). The effect of dialectical behaviour therapy on binge eating, difficulties in emotion regulation and BMI in overweight patients with binge-eating disorder: A randomized controlled trial. Mental Health & Prevention, 9, 13–18.
Randall, J., Cunningham, P. B., & Henggeler, S. W. (2018). The development and transportability of multisystemic therapy-substance abuse: A treatment for adolescents with substance use disorders. Journal of Child & Adolescent Substance Abuse, 27(2), 59–66.
Richter, P., Werner, J., Heerlein, A., Kraus, A., & Sauer, H. (1998). On the validity of the beck depression inventory. Psychopathology, 31(3), 160–168.
Saedy, M., Ardani, A. R., Kooshki, S., Firouzabadi, M. J., Emamipour, S., Mahboub, L. D., & Therapy, C.-B. (2018). Effectiveness of acceptance-commitment therapy on craving beliefs in patients on methadone maintenance therapy: A pilot study. Journal of Rational-Emotive & Cognitive-Behavior, 36, 1–15.
Serre, F., Fatseas, M., Denis, C., Swendsen, J., & Auriacombe, M. (2018). Predictors of craving and substance use among patients with alcohol, tobacco, cannabis or opiate addictions: Commonalities and specificities across substances. Addictive Behaviors, 83, 123–129.
Serre, F., Fatseas, M., Swendsen, J., & Auriacombe, M. (2015). Ecological momentary assessment in the investigation of craving and substance use in daily life: A systematic review. Drug and Alcohol Dependence, 148, 1–20.
Sharifi, V., Assadi, S. M., Mohammadi, M. R., Amini, H., Kaviani, H., Semnani, Y., & Shooshtari, M. H. (2009). A persian translation of the structured clinical interview for diagnostic and statistical manual of mental disorders: psychometric properties. Comprehensive Psychiatry, 50(1), 86–91.
Simons, J. S., & Gaher, R. M. (2005). The Distress Tolerance Scale: Development and validation of a self-report measure. Motivation and Emotion, 29(2), 83–102.
Taheri, Z., RezaeeJamaoei, H., & Zamani, S. (2019). The effect of distress tolerance education on emotional regulation and improvement of alexithymia in patients with masturbation. Quarterly Journal of Child Mental Health, 6(1), 54–69. https://doi.org/10.29252/jcmh.6.1.6.
Tang, Y.-Y., Hölzel, B. K., & Posner, M. I. (2015). The neuroscience of mindfulness meditation. Nature Reviews. Neuroscience, 16(4), 213.
Vujanovic, A. A., Wardle, M. C., Bakhshaie, J., Smith, L. J., Green, C. E., Lane, S. D., & Schmitz, J. M. (2018). Distress tolerance: Associations with trauma and substance cue reactivity in low-income, inner-city adults with substance use disorders and posttraumatic stress. Psychology of Addictive Behaviors, 32(3), 264.
Westphal, M., Aldao, A., & Jackson, C. J. M. P. (2017). Emotion dysregulation in comorbid posttraumatic stress disorder and substance use disorders: A narrative review. Military Psychology, 29(3), 216–233.
Witkiewitz, K., Bowen, S., Douglas, H., & Hsu, S. H. (2013). Mindfulness-based relapse prevention for substance craving. Addictive Behaviors, 38(2), 1563–1571.
Zhou, J., Feng, L., Hu, C., Pao, C., Xiao, L., & Wang, G. (2019). Associations among depressive symptoms, childhood abuse, neuroticism, social support, and coping style in the population covering general adults, depressed patients, bipolar disorder patients, and high risk population for depression. Frontiers in Psychology, 10, 1321.
Acknowledgments
We thank the Thalas Babajani Health Network of Kermanshah, Iran.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the Local Ethics Committee at the Kashan University of Medical Sciences, Kashan, Iran (IRCT20170314033079N3).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rezaie, Z., Afshari, B. & Balagabri, Z. Effects of Dialectical Behavior Therapy on Emotion Regulation, Distress Tolerance, Craving, and Depression in Patients with Opioid Dependence Disorder. J Contemp Psychother (2021). https://doi.org/10.1007/s10879-020-09487-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s10879-020-09487-z